When will Ireland really leave lockdown? We are succeeding in suppressing SARS-CoV-2 transmission, and people are now concerned with the developing exit roadmap, and what it will look like on the other side. These are pertinent issues, but they don’t deal with the real problem.
It’s not about how we get out, it’s about how we stay out. How will we function as a society for 12-18 months, while preventing future infection surges and lockdowns?
We are coming to the end of the ‘hammer’ phase, where our draconian suppression measures have brought the virus under control. We must now transition to the ‘dance’ phase, and keep it there until we have a vaccine. The hammer was painful and effective, but it only bought us time.
The dance is more liveable, but dancing is an active and energetic process that we must persist with, in a carefully choreographed way and without mistakes. The essential cornerstone of the dance phase is mass testing.
The strategy
We need to be able to go to work, to school, and to socialise while co-existing with this virus in the population. To do so we must have a strategy to actively maintain a SARS-CoV-2 reproduction number that is sufficiently below 1, for an extended period of time.
The scale of this problem must not be underestimated. The first Covid-19 patient entered Ireland on February 29th, when there were 85,000 confirmed Covid-19 cases worldwide. Today, there have been 3.4 million Covid-19 cases in the world, and when we come out of lockdown we can expect that there will be thousands of active infections in the Irish population.
Half of the infectious carriers are asymptomatic, yet spreading the virus in the community. Social distancing alone will not suffice.
For particular isolation to work we need to know exactly who has the virus, when they contracted the virus, and who they likely infected
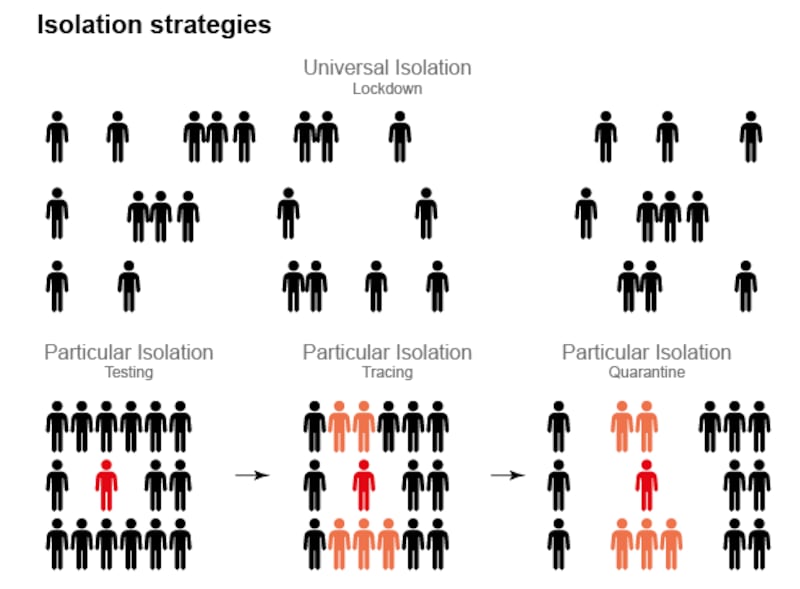
In the absence of a vaccine or effective treatment there is only one thing that can keep the virus under control: isolation. We isolate the virus by isolating the people who carry it. This is working very well so far, with the entire population in effective isolation from one another.
But we have been relying on a blunt form of universal isolation that is both all-inclusive and protracted. Everyone is effected, and for an extended period of time. As we emerge from lockdown we must transition to a sharper form of particular isolation, which would be specific and temporary.
Only people with the virus, or who are likely to carry the virus, would be isolated and this isolation would last for a limited period of time. But they must be isolated. A refined framework of particular isolation will allow the population at large to continue as normal, but it requires a crucial currency: information.
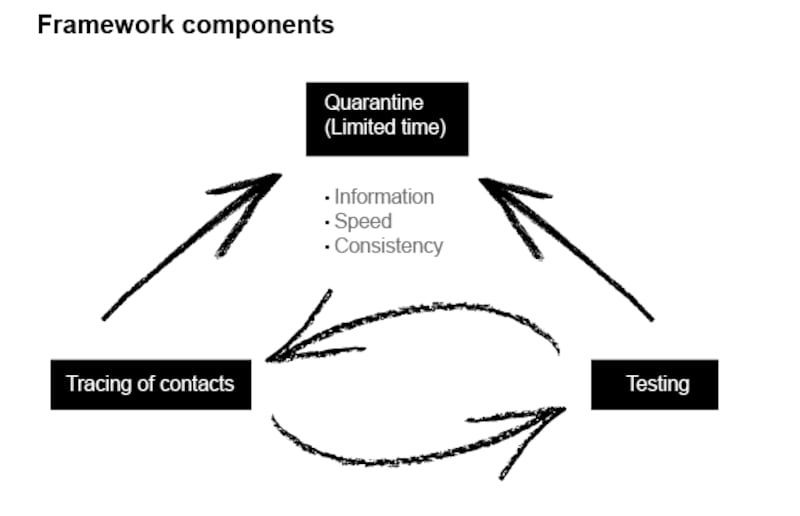
For particular isolation to work we need to know exactly who has the virus, when they contracted the virus, and who they likely infected. The information needs to be comprehensive, rapidly sourced, and reliable. We need to process this information quickly, and then employ it without delay to isolate affected individuals and their close contacts.
There is no need to reinvent the wheel here, and we should not be distracted by various untested and piecemeal strategies being employed across Europe in the coming weeks. We simply need to look at what’s been proven to work, and then adapt such a strategy to here.
We need to look primarily to Asia, and the model is South Korea. There, the infrastructure for epidemic management was so sophisticated that a lockdown was not even necessary and business continued throughout an early outbreak.
This all hinges entirely on how we manage, and maintain, this coming period of transition
The Irish Government, the European Commission, and the World Health Organisation have generally similar conditions for exiting lockdown: stable non-exponential reproduction of the virus, sufficient healthcare capacity, adequate public health education, and a testing/tracing infrastructure.
However the proportionate challenge, and importance, of the final feature of testing and tracing requires far more of our attention and investment than we are currently paying it. And we need a clear societal agreement of how testing and tracing will directly inform a strategy of particular isolation and the ensuing quarantine of suspected and confirmed SARS-CoV-2 carriers for defined periods of days or weeks.
An effective strategy requires a substantial level-up in both the scale and speed of our contact tracing and laboratory testing operations. Crucially, it will rely on centralised coordination of information and the effective isolation of all cases to prevent outbreaks.
The financial cost of such an operation is relatively modest, and it will be an excellent investment. But the organisational effort required is herculean, and the execution of such a strategy will require innovative and disruptive thinking on the part of government and the apparatus of state.
We are impatient about exiting lockdown, and we are anxious about what the new normal will look like - socially and economically. But this all hinges entirely on how we manage, and maintain, this coming period of transition. To paraphrase the late Vivien Greene, this isn’t about waiting for the storm to pass. It’s about learning how to dance in the rain.
The plan
As soon as we come out of lockdown, an operation must be in place to identify and isolate all symptomatic and asymptomatic SARS-CoV-2 carriers. This operation must be robust and sustainable for 18 months. If it falters, we will experience further infection spikes and lockdowns.
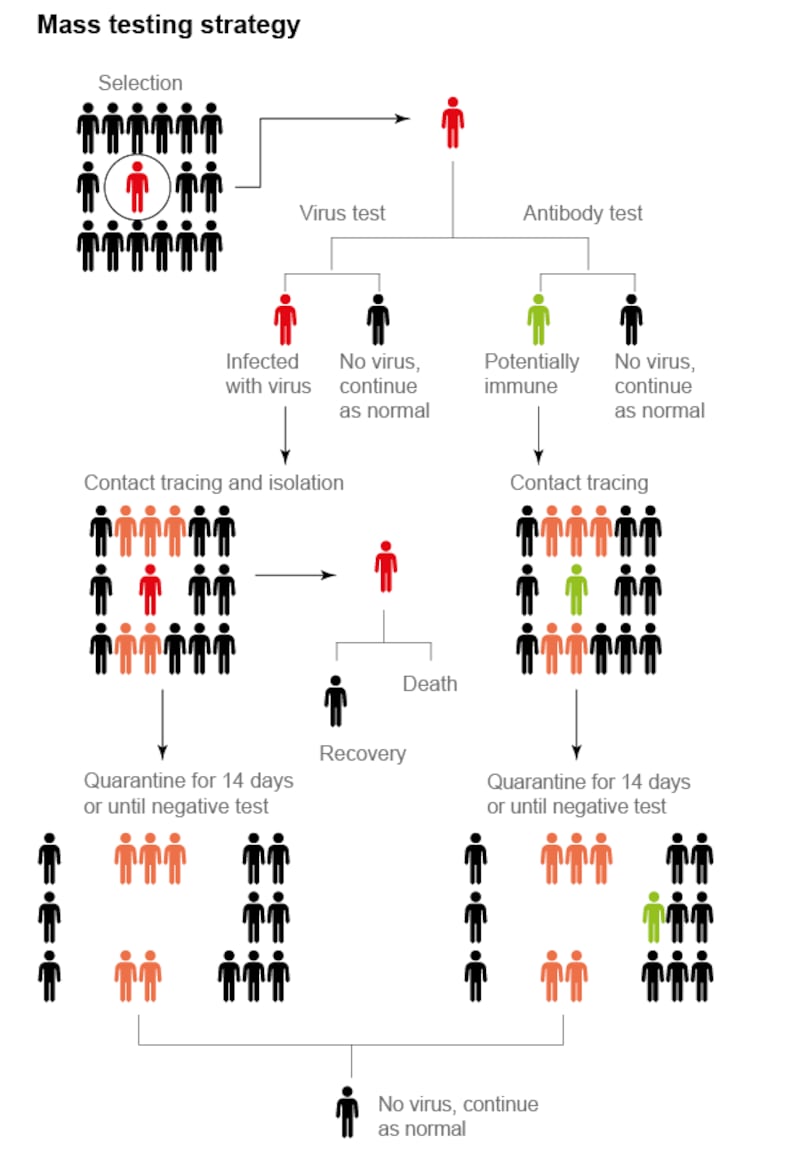
Central to a strategy of particular isolation is knowing exactly who has the virus. Mass testing is therefore the crucial ingredient. Indeed, testing has been the cornerstone of the successful South Korean exit strategy. Successful countries are conducting about 100 tests for every confirmed case.
So, if Ireland has say a total of 200 Covid-19 cases per day when we come out of lockdown, we should be conducting 20,000 tests per day. But it’s not just about capacity. As of April 28th, South Korea had performed a total of 608,514 tests (11,784 tests per million people), while Ireland had performed 153,054 tests (31,235 tests per million people).
In other words Ireland has performed nearly three times as many tests per capita as South Korea so far. What’s the difference? Speed. In South Korea, test results are texted to people less than 24 hours after swabbing. In Ireland, challenges in reagent supply and coordination have resulted in testing times ranging from many days to many weeks.
A consistent daily delivery of fast test results is crucial if the information is to be acted upon and the positive cases isolated. While under lockdown, delayed test results are still useful for estimating the prevalence of SARS-CoV-2 in the population. But for the purposes of isolating infected carriers, delayed test results are next to useless.
Over the coming weeks, we will be scaling up to a capacity of about 100,000 tests per week. But testing capacity is just a measure of the number of tests that can be performed in a lab in a given day. A more important logistical measure is testing throughput, which covers the identification of the individual, sample collection, sample delivery to the lab, RNA extraction, PCR testing, and communication of the result back to the individual.
We need a throughput of at least 15,000-20,000 tests per day with a 24-hour turnaround time from swabbing to results. To achieve this we must adapt our efforts to overcome recurring bottlenecks not just in lab-testing capacity, but in the logistical chains around it. GP referrals may be impractical, and could be replaced with central call centres followed by rapid sample collection at regional test centres or at home.
The rollout of self-testing kits, as recommended by the European Commission, could be combined with a courier system for sample delivery as saliva-based testing is refined.
Testing provides us with the primary information of who needs to be isolated in the population after lockdown. But it is only one part of the operation. It needs to be bridged with contact tracing in order to link positive cases with asymptomatic and presymptomatic carriers.
Half of SARS-CoV-2 carriers are asymptomatic, and symptomatic Covid-19 patients are infectious for 2-3 days before developing symptoms. This means that our contact-tracers are in a constant race against time to identify and quarantine contacts. All significant contacts of positive cases need to be immediately quarantined, and after the appropriate incubation period, tested themselves. If contacts test negative then they can quickly exit quarantine after a few days of inconvenience.
If they test positive, then they remain in isolation for 14 days. The contacts of the positive primary contacts (secondary contacts) would then be quarantined and tested, and so on for the tertiary contacts of the positive secondary contacts.
Recent modelling studies from Imperial College London suggest that for manual contact tracing to be successful, 20-30 contacts would need to be quarantined for every symptomatic case.
If we are seeing 200 symptomatic cases per day we would require at least 6,000 contact-tracing interviews per day to ascertain the primary contacts of symptomatic cases. This number can be reduced if we limit the number of contacts made in general, and with digital contact-tracing support.
Our manual contact-tracing operation is scalable, but for it to be successful it also must be fast. It needs to be supported by ethically managed electronic support. In South Korea, information garnered from people who tested positive includes credit card records, health records, GPS information from their phones, and CCTV footage from places they visited.
This information is then released (anonymously) so that people can see if they were a close contact of a primary case. It also allows people to avoid areas where there is a large number of infected individuals. A more moderate form of electronic surveillance involves purpose-built encrypted Bluetooth apps (such as that being developed by the Health Service Executive), which keep records of all individual contacts, giving notifications when people test positive.
This approach reduces privacy concerns but it is only effective with extensive buy-in from the population: for Bluetooth tracing to be effective, research shows that they need to work on an “opt-out” policy rather than an “opt-in”. There will be a central trade-off between manual contact tracing and electronic information use. The more we rely on manual tracing, the more state agents will need to be involved and the more contacts will need to be pre-emptively quarantined.
Relying more on electronic surveillance, as in South Korea, greatly increases the effectiveness of contact tracing, but raises ethical questions of privacy.
Random testing of individuals in the population should be a central component of the operation. This should include extensive antibody testing on top of virus testing, to estimate how many people have previously been infected and whether they are immune (note: it is currently unproven whether infection confers immunity, but it is likely).
Weekly screening of all healthcare workers and at-risk groups should be conducted regardless of symptoms or contacts, as this has been estimated to reduce their contribution to transmission by 30 per cent.
Testing throughput needs to be at 24 hours, with subsequent contact tracing completed within a 48 hour window
Besides the active searching measures of testing, tracing, and isolation; broader ‘passive’ measures will surely be required to help maintain an acceptable reproduction number. Travel restrictions will certainly be necessary to prevent new cases from entering the population. All arrivals should be required to quarantine for two weeks regardless of citizenship. A rapid airport testing facility for essential travellers may be appropriate, and could potentially be scaled up for all travellers. And we need to be wearing masks.
The Implementation
How will we implement an exit strategy and the operational logistics required of it? The strategy of particular isolation requires a large, fast, and sustainable operation of testing, contact tracing (manual and electronic) and targeted isolation of positive cases with quarantine of all close asymptomatic contacts. How do we get this done?
We have an opportunity in Ireland to get this right. We enacted lockdown early, and with the right exit strategy we can minimise the overall damage to the country. Being an island, we can more effectively contain the spread of Covid-19. We have the core technical components in place - a large potential laboratory testing capacity, an evolving logistical chain for testing throughput, and a scalable contact tracing operation.
What elements are missing from our overall operation? The first is speed - we’re currently far too slow. Testing throughput needs to be at 24 hours, with subsequent contact tracing completed within a 48-hour window. The second is information, everything depends on knowing who is positive and which contacts to quarantine.
This requires electronic contact tracing and real-time centralised coordination between testing sites, contact tracers, and central governmental agencies. The third is consistency; we need to be able to maintain a robust operation on a daily basis with all the required materials and reagents. And finally we need strategic, scientific leadership.
The task at hand is very achievable. It has worked in many other countries, and we have everything we need to do it here. But it requires an industrial mind-set in implementation, and a much more developed scientific orientation to guide political leadership. Despite the immense and tireless efforts of many dedicated individuals, it’s clear that central structural change is urgently necessary to put a functional operation in place, and to keep it in place for 18 months.
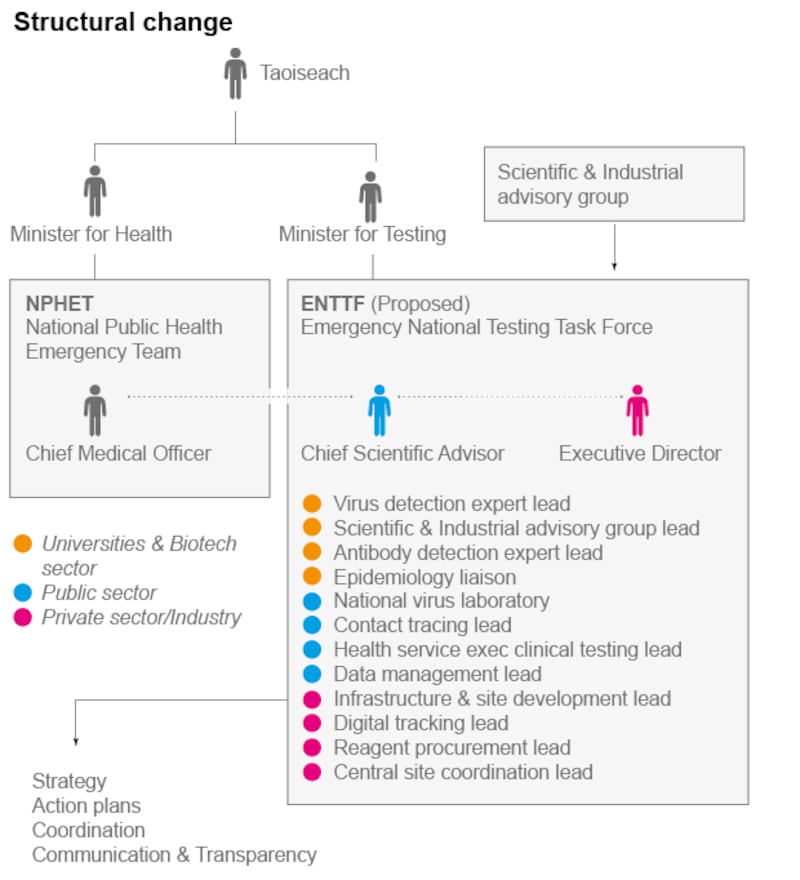
The UK’s Scientific Advisory Group for Emergencies (Sage) has been criticised for being over 50 per cent government advisers with only a minority of independent scientific experts. Our National Public Health Emergency Team (NPHET) is nearly 100 per cent Department of Health and HSE official staff.
The supporting Expert Advisory Group contains mostly medical doctors, and a handful of clinical academics. A subsidiary research subgroup holds 10 other advisers, less than half of whom are active research scientists.
Altogether, this structure represents a very narrow band of scientific knowledge, with the actual experts isolated from policy-makers by multiple degrees of separation. Successfully controlling the Covid-19 situation in Ireland requires a diverse base of our most established scientific experts to be communicating directly with politicians on a regular basis.
There are existing roadmaps. The South Korean Covid-19 playbook is a proven strategy. Harvard University has published a Roadmap to Pandemic Resilience. The Tony Blair Institute for Global Change has produced a series of papers of how to organise a testing/tracing operation that is particularly relevant to Ireland. They all emphasise massive testing, contact tracing, isolation - and the resources required to act quickly.
Meeting this challenge requires central organisational changes that utilise outside help and expertise, by identifying people with specific skill sets and putting them in the right places. Our society is full of knowledgeable, talented, and resourceful citizens who are deeply motivated and able to help. They are to be found in the private sector, in biotechnology, the pharmaceutical industry, and in academia. These are people not normally employed within the frameworks of the Department of Health and the Health Service Executive, but who offer different and complementary skill sets and expertise.
An effective emergency national testing task force would require political legitimacy and empowerment. A senior Minister for Testing would have the ability to make rapid decisions as the situation evolves, in daily direct contact with the Taoiseach. This task force would be led by a senior scientist (for example, the Chief Scientific Adviser) and an Executive Director from the private sector. It would include industrialists, scientists, and managers in testing, tracing, and data management. It would work strategically - informed by the most current international scientific knowledge, with the pace and capacity of the commercial sector, but with the legitimacy and authority of state. For public confidence, it would work in a transparent fashion following the New Zealand model.
This infrastructure would be an excellent investment. There was no Covid-17 or Covid-18, but there could be a Covid-21 or Covid-25. A comprehensive infrastructure allowed South Korea to manage their Covid-19 outbreak without business closure. Developing our own structures will enable us to function in the face of future pandemics, without suffering lockdowns or waiting for vaccines.
The model of South Korea is the best fit for a democratic society such as Ireland. For this to work, it requires our central testing infrastructure to incorporate leading individuals and best international practices from the private sector. But it also requires the active citizenship of everyone in the population. We need to comply with moderate social distancing until we have a vaccine. We need to observe assiduous standards of hygiene and public behaviour. We need to avoid large social gatherings. We need to adapt our work and school environments to reduce transmission risks. We need to comply with a certain degree of responsibly managed electronic surveillance. We need to wear masks. But everyone could go to work again. Schools would open on reduced schedules, and exams would happen. People could socialise in a reasonably normal way. This could quickly evolve into a pace of life that would be both liveable, and economically productive, for the coming 18 months.
Our economy, education system, and wellbeing all hinge on the success of our exit strategy. Whatever our exact operational structure, it needs to be in place the day lockdown ends. The clock is ticking.
Tomás Ryan is associate professor in the School of Biochemistry and Immunology at Trinity College Dublin and Chair of the European FENS-Kavli Network of Excellence














