
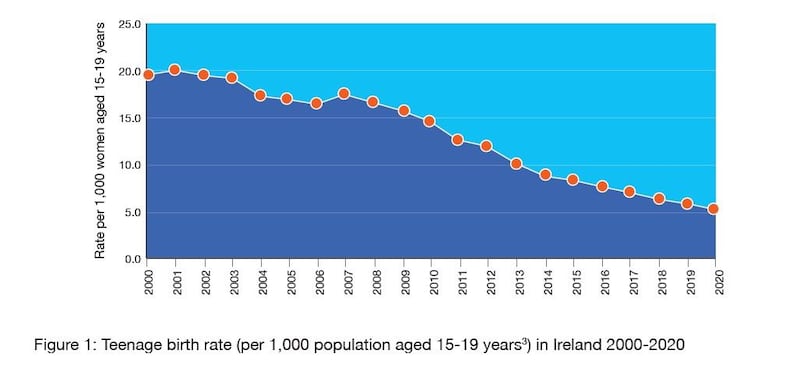
A dramatic 73 per cent fall in the number of births to teenage mothers in Ireland over the past 20 years is a lone statistic, but one that reflects many strands of societal change.
No single factor can explain this downward trend but a new document, Information Summary about Teenage Pregnancy in Ireland 2000-2020, to be published by the Health Service Executive (HSE) this week, takes a research-based look at how it has been achieved. It is something to be celebrated because this sort of positive development often goes under the radar when public focus tends to be on what’s going wrong with everything, rather than what’s going right.
Of course, not every teenage birth is a negative experience for all involved, but documented evidence and common sense indicate that such early parenthood is a monumental challenge, with the risk of adverse outcomes, and so best avoided.
Teenagers in Ireland today are more likely to remain in education and more likely to make healthier lifestyle choices than in the past
In the first year of the new millennium, 3,116 births to teenage mothers were recorded, according to the Central Statistics Office (CSO). By 2020, that figure had dropped to 830. In percentage terms, teenage births represented 5.7 per cent of the 54,789 births in the Republic in 2000; in 2020, they accounted for just 1.5 per cent of the 55,959 births that year.
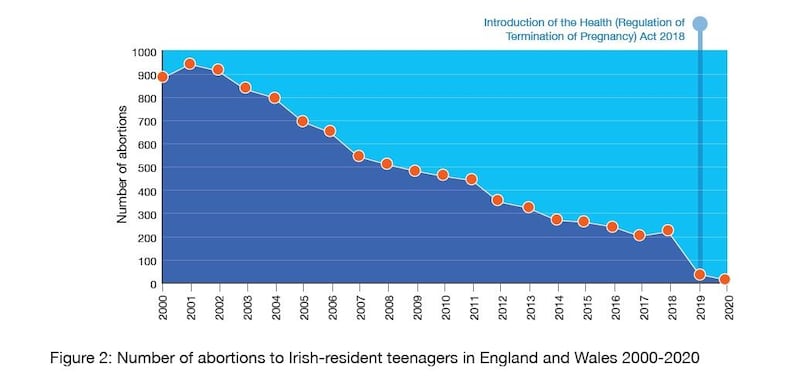
It’s not the case, as some might suppose, that more pregnant teenagers were opting for abortions because there has been a sharp downward trend there too. In 2018, 218 Irish-resident teenagers used abortion services in England and Wales, compared with 884 in 2000. That is a decrease of 75 per cent. (An age breakdown is not available of the 6,577 women who had abortions in the Republic in 2019, the first year after the introduction of the latest abortion legislation here.)
The HSE document also refers to the unknown numbers of people buying abortion pills online before the changes in legislation. But it cites a study in which one online provider of these pills reported consultations with 5,650 women from the island of Ireland over six years between 2010 and 2015, of whom 4.6 per cent were under the age of 20.
Teenagers can be stigmatised in a particular way, says Maeve O’Brien, interim programme lead with the Sexual Health and Crisis Pregnancy Programme (SHCPP), in an interview with The Irish Times. “But when you look at the data, they’re doing brilliantly because they are being supported to do so and we just wanted to make that point.”
She and her team in the health and wellbeing section of HSE strategy and research tracked and analysed the figures for teenage births. This summary of their findings, available on sexualwellbeing.ie, concludes that "teenagers in Ireland today are more likely to remain in education and more likely to make healthier lifestyle choices than in the past".
Eighty per cent of sexually active 17-18 year-olds always use some form of contraception and about 90 per cent use it the first time they have sex, according to findings from the Growing Up in Ireland longitudinal study. Indications of more responsible behaviour from other studies include the percentage of 10-17-year-olds who reported ever having been drunk falling from 32 per cent in 2002 to 19 per cent in 2018, and the rate of smokers in that age group dropping from 18 per cent to 5.3 per cent over the same period.
The explanation for the reduction in teenage pregnancies is complex and multi-factorial, says O’Brien, and it’s also part of a global trend. “But the key point is that there have been broad policy, legislative and societal changes in Ireland in the last 20 years that have contributed to a supportive environment.”
Here we look at some of the factors at play over the past two decades in the proverbial “village” that it takes to raise a child.
More sex education
Relationships and sexuality education (RSE) isn’t something that just happens in schools, but the introduction of an RSE curriculum within the education system back in 1996 has had an accumulative effect.
“Evidence shows it is having a positive effect where young people are getting it and people think the quality of it is good,” reports O’Brien.
However, ensuring consistent delivery and quality of such teaching is still a work in progress, as acknowledged by the current review of RSE provision being undertaken by the National Council for Curriculum and Assessment, within the broader context of Social, Personal and Health Education (SPHE) across both primary and secondary schools.
It is more critical than ever that teenagers receive clear, factual information about sexual health and contraception
O’Brien praises “excellent partnerships between statutory and community providers” that aim to support people to improve their health and wellbeing generally, of which sexual health is a part.
“Young people need safe spaces, they need supportive, trustworthy adults around them,” she says. In working with schools, youth organisations and parents, the SHCPP is trying to ensure appropriate information is conveyed to young people in a supportive way.
The medical director of the Irish Family Planning Association, Dr Caitríona Henchion, says it's clear from its services that teenagers are more aware that they need to protect themselves from sexually transmitted infections (STIs) as well as unintended pregnancy.
“However, misinformation about sexual health among teenagers is still very common,” she continues. “It is more critical than ever that teenagers receive clear, factual information about sexual health and contraception so that they are empowered to be safe and healthy if they are in a sexual relationship.”
Parenting changes
Criticism and debate about RSE tends to focus on schools but they complement rather than replace the parents’ role, says O’Brien, whose programme has also identified a “cultural component” in Ireland to parent-child communication about sexual health.
“A lot of parents said they got nothing when they were children, but they really wanted to change this for their own children. But when it came to doing it, they still lacked confidence and they were concerned about transgressing the norms of other parents.”
This demonstrates a shift in attitude towards talking to children about sexuality but also legacy issues. “There’s a desire to do it, which wasn’t there in the past, but we are still being prevented in some way by our past,” says O’Brien.
Now contraception is an early and active suggestion by parents to their teenagers as they see the drawbacks of an unwanted pregnancy
What used to be referred to as “the talk” – although ideally it should be a series of age-appropriate discussions over a number of years – doesn’t have to be focused on sex. “It’s having conversations about puberty and linking that to becoming an adult and what that means,” she says. But parents’ discomfort is still problematic.
Some 45 per cent of young people have discussed sex and relationships with parents by age 13, according to Growing Up in Ireland data, and that rises to 60 per cent by age 17. “But that leaves 40 per cent by age 17 that hadn’t. So there’s still a bit of work there,” she remarks.
However, today's parents are more likely now to be leaving boxes of condoms in teenagers' bedrooms rather than books about "growing up" as their parents did, suggests Aileen Hickie, chief executive of Parentline. This confidential support service is 40 years old this year and has seen "a vast change in attitude" among callers.
Parents in the past were generally horrified at the idea of suggesting contraception to their daughters as they believed that would encourage promiscuity, she says. “Now it is an early and active suggestion by parents to their teenagers as they see the drawbacks of an unwanted pregnancy and are more accepting that their child is sexually active.”
Easier access to contraception
Contraception has become much more available to teenagers over the past two decades and the range of options has also increased. The situation will be further improved by the introduction this August of a scheme, funded in Budget 2022, to provide free contraception to all young people aged 17-25 years.
Wider use of of long-acting reversible contraceptives (LARCs) has been indicated as a factor in the reduction of teen pregnancies in the UK. However, the Irish Family Planning Association says that in the absence of robust up-to-date Irish data on the use of contraception by sexually active adolescents, it can't confirm that LARCs have contributed to the decline in teenage pregnancy here.
However, LARCs provide a “fit and forget” option, and are considerably more effective than user-dependent methods such as the pill or the condom, says Henchion. With the high upfront cost of this method being a barrier for some, the new scheme will remove cost as a consideration from contraceptive decisions for 17-19-year-olds. But, she adds, “the IFPA strongly believes there should not be a lower age limit on this scheme, so that younger teenagers are not left behind”.
Prof Abbey Hyde of UCD school of nursing, midwifery and health systems, who led the first comprehensive study of teenage sexuality in Ireland in 2004, says research at that time found inconsistent use was a huge problem for those who used contraception, especially if they were under the influence of alcohol.
Wider use of emergency contraception since then may be one of the many contributing factors to fewer teenage pregnancies. Access to the so-called “morning after pill” was made easier here in 2015 when it became available without a prescription.
Although, Hyde points out, this would only account for teenagers motivated to act by the belief that they might be pregnant. There was evidence from previous studies of a lack of “agency” about preventing pregnancy among young people who came from a background of culturally and socio-economic disadvantage.
“It wasn’t that they went out to get pregnant, it’s rather that they drifted in because of this general milieu, their set of circumstances, meant they weren’t active agents over any part of their lives, let alone fertility.”
Increased educational attainment
The rise in the numbers of young people staying in school to complete their Leaving Cert and going on to third-level is regarded as a significant factor. Higher levels of education have been shown to contribute to improved health generally and are linked to protective behaviours.
Irish research suggests that those who leave school by age 17, or who have lower levels of educational attainment, are more likely to report having sex before they reach 17, and are more likely to experience a crisis pregnancy.
Of those pupils who started secondary school in 2014, 91.5 per cent stayed in school to complete the Leaving Certificate, compared with 78.3 per cent who entered first year in 1994.
Unplanned pregnancy can happen to any young person, but teenagers for whom the future seems most uncertain remain the most vulnerable
This increase in school retention "feeds into less teen pregnancy because research shows that the more you have to lose in terms of your life plan, the more careful you would be around contraception", explains Margaret Morris, national coordinator of the Teen Parents Support Programme.
With that comes the “cumulative idea of norms shifting”, says Hyde. When young people look around their neighbourhood, they are less likely to see their peers becoming pregnant.
Unplanned pregnancy can happen to any young person, but teenagers for whom the future seems most uncertain remain the most vulnerable. These include youngsters living in, or having just left, State care and also those growing up in acute socio-economic disadvantage.
The SHCPP has worked closely with Tusla on how to address the fact that so many young people leaving care were parents by their early 20s at the latest, says O’Brien. She also commends HSE colleagues for the healthy communities initiative, which focuses on the most deprived areas.
Not for a minute, she adds, is the SHCPP suggesting that the fall in teenage pregnancy is an indicator, by itself, of good adolescent health or “that our work here is done. We are very aware that teenagers are constantly facing new and different challenges. We will continue to try to address these as they evolve.”
National support programme
Early parenthood in Ireland may be falling but a national support programme for teenage parents is still only able to reach about 25 per cent of them.
The Teen Parents Support Programme, run by Treoir, the national federation of services for unmarried parents and their children, has 11 projects around the country. But it wants additional resources to expand its operations.
“Ideally, we would like all teen parents to have this kind of support,” says the TPSP national co-ordinator Margaret Morris. There is no dispute, she says, about the effectiveness of the long-term, consistent support they offer, from pregnancy right through to when the child reaches two years of age – and beyond in some circumstances.
She has been working in this field for almost 17 years and has observed a “wonderful decline” in numbers of teenage parents.
“Hopefully, this will continue because unless a young parent gets very good support, whether it’s from an organisation like us, or from the family and from school, their life chances and the life chances of the child are hugely reduced. There aren’t that many of them now so we should be able to support all of them.”
In her experience, families rally around teen parents, particularly the grandmothers. That’s not to say there isn’t usually an adaptation period of coming to terms with the idea, when there may be anger towards both the young woman and the father. Also, some are very stretched in what support they can provide.
The significant change Morris has witnessed over the years is the attitude of schools, which have been much more supportive.
We are getting referrals from hospitals, Tusla and other social services asking us to support this group who are not teenagers, but still extremely young
“I think they see it less now as a reflection of the school as they might have 20 years ago. I would see a big shift there but I think families have always done their best.”
More than half the teenagers are referred to the TPSP by maternity hospitals, others by Tusla, GPs, youth organisations and schools. She welcomes that fact that most come to them antenatally.
There is no other comparable service for teen parents, says Morris, as they work with them “where they’re at as young people”. They can be scatty and inconsistent, like all teenagers, and she believes their staff are very good at dealing with that.
However, she acknowledges the achievements of organisations such as Tusla, who get a bashing all the time. Tusla's School Completion Programme has succeeded in keeping at-risk youngsters in education and it also deserves a lot of credit, she says, for its Prevention Partnership and Family Support work. Wider health education as promoted by the HSE, has also helped.
Yet, there are still many vulnerable young parents that Morris would like to be able to reach. “There are areas in Dublin, such as Clondalkin, where schools have asked for a TPSP programme and there isn’t one.”
The TPSP would like to be able to increase its work with teenage fathers and also extend its services to parents under 25.
A woman having a baby at age 20 or 21 is now very young in societal terms, Morris points out, since the average age for a woman giving birth is 33.1 years, according to CSO figures from 2019. “We are getting referrals from hospitals, Tusla and other social services asking us to support this group who are not teenagers, but still extremely young.”











