Congestion. Sinus headache. The “Covid voice”. A general feeling of tiredness. Constant throat-clearing. Skin sensitivity. Fewer temperatures. Fewer coughs. And far higher rates of transmissibility.
GPs in some of the country’s Covid blackspots are noticing a marked change in the early symptoms during the third wave, which has seen Ireland leapfrog from one of the least-affected countries in Europe to the worst-hit in the world.
Information is still emerging about the new strain, B117, which was first detected in the UK and was recently estimated – based on 317 samples – to be present in around 45 per cent of cases here.
The World Health Organisation’s emergencies chief, Mike Ryan, said last week that it is “increased social mixing”, and not this new variant, that has caused the dramatic surge in infections.
However, what we do know is that it is significantly more transmissible. The South African variant – thought to be even more transmissible – has also been found in the Republic. And the experiences of GPs in some of the country’s worst-hit areas for Covid-19 suggest that the virus may now also be presenting differently from the way it did during the first wave.
Here, GPs on the frontline of the world’s worst outbreak share their stories.
Cavan-Belturbet, Co Cavan
‘This is completely different to last March’

Over the Christmas period, between December 22nd and January 4th, the Cavan-Belturbet electoral area – home to just under 26,000 people – had an infection rate of 986 per 100,000. That figure is now 1,621 per 100,000.
“It’s carnage out there,” says Dr Dara Hume, a GP in the Drumalee family practice. “People’s attitude is very different. And we’re finding work very difficult from that point of view. People are fed up being told what to do, or what they can’t do.
“Unfortunately, people do not realise this is completely different to last March. They’re almost angry at us for referring them. They think: ‘I haven’t gotten it this far, I’ve been okay so far.’ Or someone they knew had it and ‘it’s only a cold’. I don’t think people are aware that it’s a completely different ballgame now. This variant has changed everything. It is so contagious.”
Doctors in her practice are hearing a lot of, “‘It’s just a cold. It’s just my sinuses. It’s my usual.’ It’s proving quite difficult to convince people that what they think is a sinus infection is probably Covid. Everything new is Covid until proven otherwise. Lots of patients don’t have temperatures. Lots don’t have coughs.”

Still, many people are reluctant to get tested. “We’ve had a lot of patients refuse to bring their children for testing” because of the implications for the rest of the family.
There has been no real let-up in calls this week, despite Christmas socialising having stopped. “I have no sense it’s slowing down at all this week. It’s the ripple effect. It’s like you throw a stone into a pond, and as each ripple goes out, it starts the next ripple.
One older patient had only been to Tesco, and wore her mask the whole time. But she still got sick, tested positive, and died recently
“The vast majority of the phone calls from people with symptoms are contacts of contacts. They’re saying ‘my brother has been a contact’ or ‘my friend rang me and said they are a contact’. We need to be much more vigilant on any new symptom – which would include runny nose, all the facial pains you get with sinusitis.”
One other worrying trend she has noticed is that “our most ill patients now are in their 50s and 40s. Nobody really knows why that is. It’s often people without underlying conditions.”
It’s hitting them, she says, “in the second part of their illness. The typical thing is flu-like symptoms for a couple of days, and people think they’re getting better. And then day seven, eight or nine... wham – the shortness of breath seems to kick in. And that’s quite scary.”
One older patient had only been to Tesco, and wore her mask the whole time. But she still got sick, tested positive, and died recently.
One key message that Dr Hume would like to get out is that people should ask themselves every time they leave the house: “Do I have to go out? Do I have to get my car washed? Do I have to go to the shop again? Do I have to go to a hardware shop just to pass the time?”
Belmullet, Co Mayo
‘We seem to have an Irish-style bubble’
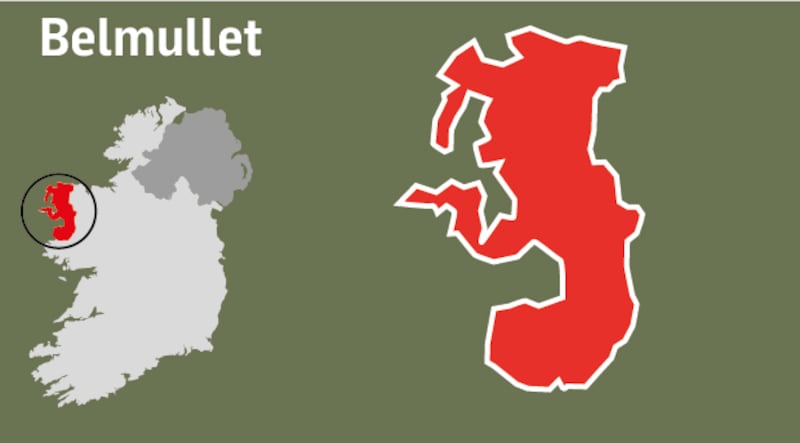
There were 11 ambulances in Belmullet last Sunday, transporting Covid patients to Mayo University Hospital in Castlebar, says Dr Keith Swanick.
He has sent up to 10 more patients to hospital since. “None of the patients I sent away were from any nursing home. They were all aged between 37 and 75.”
The area ranked as the worst-hit in the country over the two weeks up to January 4th, with one in 50 of the population struck by Covid-19. It has since risen to three times that level. Dr Swanick was so worried that he recently made a public appeal for a curfew to be introduced.
The weekend after Christmas “was really when things went crazy”, and there has only been a slight easing since. “On January 5th, we had 200 referrals. Last Monday, we had 60 referrals. People don’t have to have a cough or shortness of breath. It’s really varied now. It might be fatigue, a little sore throat, sinus symptoms. Some people have diarrhoea.

“You have to keep your antennae attuned. Even when you’re having a conversation with somebody over the phone, they might just have a little dry cough” – he makes a sound like clearing his throat – “mid-sentence, and that might be enough to refer them. And they are shocked when they come back positive.”
He’s worried that if the numbers start to come down, people will relax again. “We seem to have an Irish-style bubble. ‘They’re in my bubble. And these neighbours of ours are in the bubble too.’ All of a sudden three or four families are in a bubble.”
"A dirty glove is worse than a dirty hand. Or wearing your mask under your chin and then pulling it up to your face and taking it back down again"
The very high transmissibility of the B117 strain first detected in the UK is definitely a factor, he suspects. “I saw it here firsthand with the influx of UK people, prior to the major socialisation over Christmas. I don’t think we know enough about the new variant yet. The scientific people are afraid to say that too loudly, because they don’t want to frighten the bejaysus out of people.”
He cites a typical example of a patient living alone and having her shopping delivered by a neighbour to inside her door, as an example of how infectious the virus can be. “The vulnerable person is sitting inside the porch four or five metres away. The person who’s delivering the shopping drops it inside the porch. They’re asymptomatic. And the vulnerable person catches it. I’ve heard loads of those kinds of stories.”
The other thing we need to be more aware of, he says, is mask and glove hygiene. “A dirty glove is worse than a dirty hand. Or wearing your mask under your chin and then pulling it up to your face and taking it back down again. We need to learn how to wash masks or dispose of them.”
Adare-Rathkeale, Co Limerick
‘A lot of the symptoms are not on the referral criteria’

“GPs are at the coalface. We’re putting out fires. We have been called upon by the HSE at every stage of this pandemic to be the first port of call for our patients, which we have done,” says Dr Cathy Brogan, a GP in the Adare-Rathkeale electoral area, which recently had 2,010 positives per 100,000 population. In figures released on Thursday this had risen to 3,118 per 100,000.
“We’re at the epicentre here. In the 15 years I have worked at Rathkeale, I have never experienced such a disproportionate spike in viral infections compared to the rest of the country.
“Fifty per cent of the people getting tested here are positive, but we know our numbers are much higher, because many people with symptoms are simply refusing to get tested. They don’t want to be told they have to self-isolate.”

Dr Brogan doesn't want to speculate on the causes, but sources in the area point to an influx of visitors from the UK and other parts of Europe over Christmas, and higher levels of socialisation in both Rathkeale and Adare. The result, Dr Brogan says, is that "we're seeing practically nothing else but Covid now in this area."
The new B117 strain “doesn’t make people any sicker,” she says, but, because it’s more transmissible, “we are seeing huge numbers actually ill with it, some very debilitated. Now we are seeing deaths and morbidity at a local level which we didn’t see in the previous waves.”
She adds: “Patients are presenting with a myriad of symptoms, a lot of which are not on the referral criteria.”
"We're still getting huge numbers of positives every morning. So we'll see a lot more of that in the future"
GPs in other parts of the country have already been vaccinated, but here, in one of the worst-hit areas in the worst-hit country in the world, they’re still waiting. The mood among doctors in the area is one of stress and utter exhaustion. “The HSE have yet to let us know a date for when our team will be vaccinated.” says Dr Brogan.
“We’ve no guidelines about how to treat Covid in the community.”
On top of that, “embolic events – such as clots in the lungs and other organs – are one of reasons that people are becoming very ill and require admission. We’re starting to see ‘long Covid’: people with ongoing shortness of breath and chronic fatigue; some with myocarditis [inflammation of the heart muscle] and nephritis [a condition affecting the kidneys]. And we’re still getting huge numbers of positives every morning. So we’ll see a lot more of that in the future.”
Ballybay-Clones, Co Monaghan
‘We are calling it the Covid voice’

The electoral district of Ballybay-Clones in Co Monaghan, an area of 17,000 people, was hit by a “perfect storm” over Christmas, which saw the infection rate climb to 1,675 per 100,000 people – and this week to 3,054 per 100,000. It has been caused, says local GP Dr Jack Crummie, by “a combination of different events”.
“People were fatigued and, coming up to Christmas, they felt they deserved a bit of a get-together.” The community had avoided being hit hard in the first waves, so there were low levels of antibodies.
During the third wave, “whole families are coming back positive.” He also noticed a shift in the pattern of early symptoms: severe headache, feeling cold, tiredness, nasal congestion. “People are saying, ‘I feel it’s just a cold.’ But there’s no other flu-like illness out there.”
The people most at risk are the ones who seem to get better at around five to six days, and then experience a sudden deterioration
Fifty per cent of positive cases at Dr Ilona Duffy’s Monaghan practice over two days recently presented with nasal congestion. “We are calling it the Covid voice – not just a little sniffle, but that sinusitis, blocked nasal sound. Symptoms are beginning earlier, maybe three days after exposure.”
She believes there has been “a little of a stabilisation of things” in the area this week. “The good news is that people have really gotten a fright and changed their behaviour. But the bad news is that we are absolutely getting more calls from people who are really sick. And we have four patients in hospital at the moment. We’ve two in ICU. It’s worse than the very beginning, because these are people who are younger.”
The people most at risk are the ones who seem to get better at around five to six days, and then experience a sudden deterioration, she says.

The message she wants to get out is that “most people may be all right. But we can’t predict those who will be really sick, or who will end up with long Covid. It’s a lottery.”
Dr Crummie’s appeal to people is “return to your behaviour back in March”. The virus needs to come down to allow vaccines to be delivered in a safe environment.
Tramore-Waterford City West, Co Waterford
‘Fever hasn’t been a huge factor among our patients’

The seaside town of Tramore and Waterford City West had an infection rate of 1,010.2 per 100,000 over Christmas. The latest figure is 3,106 per 100,000.
Five per cent of the patients in one practice, the Tramore Medical Clinic, were infected with the disease. One of the practice’s GPs, Dr Austin Byrne, says the numbers of those being referred for testing fell this week to a quarter of their recent levels, so he believes the worst has passed in terms of case numbers.
The new variant may have played a role in the surge, but “if we hadn’t had a Christmas and we hadn’t got together, we wouldn’t see it in this magnitude”.
“We had a particularly strong local cluster. We had people coming from multiple public space gatherings, and a large number of spreading events. The secondary household attack rate is 70 to 80 per cent – meaning if one person gets it, 70 to 80 per cent of the family will get it too.”
"My instinct is that our absolute numbers have peaked. But our level of risk has not peaked"
The typical symptoms of cough and loss of taste are still being reported by patients, but “most cases of Covid will not present in the archetypal fashion”.
Among 20- to 40-year-olds, he is seeing a wider range of symptoms, including “head colds, aches and pains, skin sensitivity and upper respiratory symptoms. Fever hasn’t been a huge factor among our patients.”

The disease is still spreading within families, he warns. “My instinct is that our absolute numbers have peaked. But our level of risk has not peaked.”
And while for younger age cohorts “it’s mostly self-limiting and mild, people need to continue to be very careful of the over-65s. The main risk is from spread within friends and family groups.”
But there is light at the end of the tunnel, he says. Along with other GP practices in Waterford, staff at his practice were vaccinated last weekend at University Hospital Waterford. “The vaccine is coming and we will see a rapid fall-off in the hospitalisation and death rate.”

















