1) What is the flu?
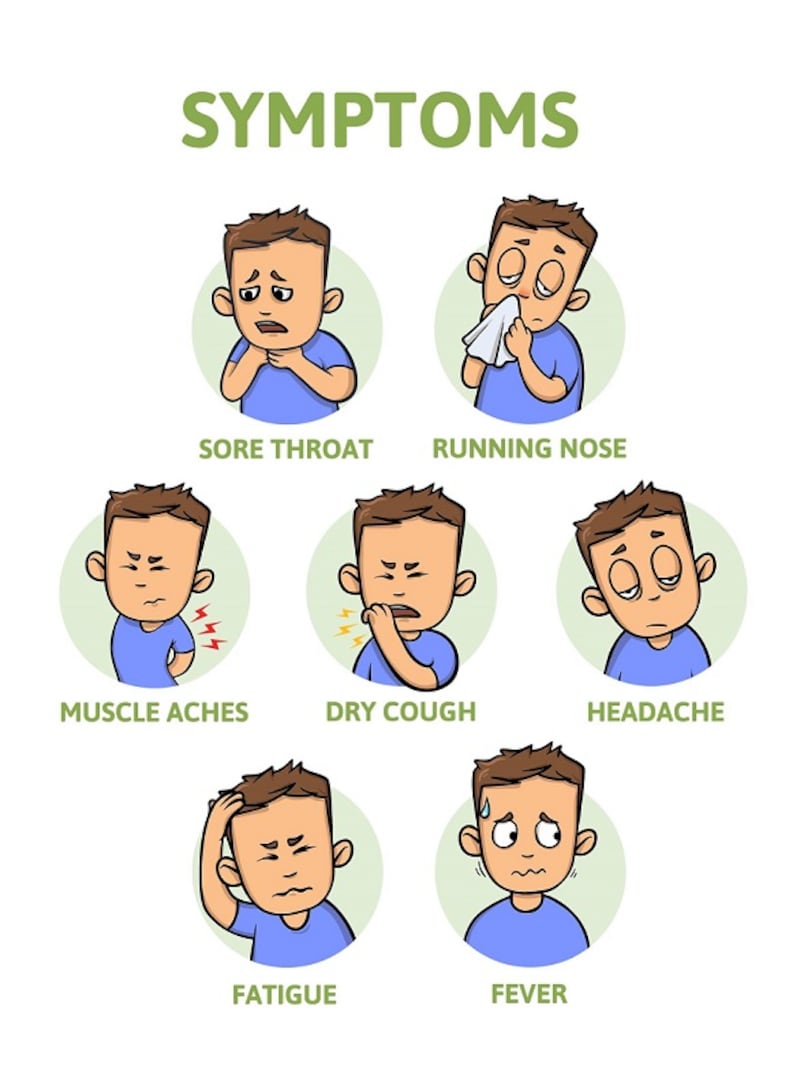
Known as influenza, seasonal flu is a highly infectious illness caused by the flu virus. It infects your lungs and upper airways, causing a high temperature and aches and pains, headache, weakness and exhaustion.
2) How dangerous is the flu?
Influenza is a serious infection and most people will be ill in bed, feeling miserable for about a week, says Dr Kim Roberts, virology lecturer and leader of the Influenza Research Group at Trinity College Dublin.
"However," adds Clonakilty GP Dr Fiona O'Reilly, "the flu can leave you exhausted and with aches and pains and a chronic dry cough for up to six weeks. "For some people," she adds, the flu can even result in chronic fatigue syndrome. Many patients also suffer from low mood after catching the flu.

And for some the flu can be fatal. In Ireland it's estimated that 200-500 people die from influenza every year. Over 2017-2018 – which, says Dr Roberts, was considered to be a severe flu season – 255 people died and 4,713 people had to be hospitalised as a result of influenza infection.
During the 2018/2019 flu season, 3,217 people were hospitalised as a result of influenza. “The flu can increase the incidence of heart attack and stroke, and lead to life-threatening complications such as pneumonia,” Dr Roberts warns.
3) How is it spread?
“One of the difficult things with flu is we can spread the virus before we know we’re sick,” says Dr Roberts. “The flu virus is released through the air droplets we generate when we breathe and talk, so about a day before symptoms start we can be spreading the virus to others. Later on in the infection we may be coughing or sneezing, which can also spread the virus.”
4) Who should get the flu vaccine?
This is an important issue. According to recent research by Boots pharmacy, which recently announced the commencement of its annual flu vaccination service, more than half of the people in Ireland have never been vaccinated against the flu – with 52 per cent of those surveyed not planning on getting vaccinated for the 2019/20 flu season.
According to experts there are a number of at-risk categories who must be vaccinated:
– People who are at most risk include those over the age of 65, as well as people with long-term medical conditions such as diabetes, chronic heart disease, asthma, chronic lung disease, cancer, or people with impaired immune systems. “In other words, people who are at risk of becoming extremely ill if they get the virus should be vaccinated,” says Dr Roberts.
– Children with long-term medical conditions should also receive the vaccine, either from their doctor, or, once they are over the age of 10, they can be vaccinated by the local pharmacist.
– Healthcare workers – from dentists to nurses, hospital porters to cleaners – should get the flu vaccine, says Dr Roberts. “Anyone dealing with members of the general public who are ill are thought to be 10 times more likely to be exposed to the flu virus. These workers should get the vaccine both to protect themselves but also to prevent the transmission of the flu virus to the patients they come in contact with.”
– Anyone who cares for or lives with someone who is in an at-risk group should get the vaccine both to protect themselves and also limit the transmission of the virus to those around them.
– People who are self-employed or who travel abroad frequently should definitely consider vaccination, says Dr O’Reilly, who warns that a bad case of flu can leave some patients feeling severely under the weather and even out of work for up to six weeks. “If you’re self-employed you may not have illness benefit. If you’re travelling abroad you may be very exposed to the flu virus either in another country or through the air on board your airplane. The air is continually re-circulated, meaning that air passengers infected by the virus can quickly spread it to other passengers as this is an airborne condition.”
5) What the vaccine does and doesn’t do
The flu vaccine does protect many people from the annual flu, but it’s not perfect. “On average it is 60 per cent preventative,” says Dr Roberts. “The vaccine changes from year to year because the virus changes every year – but it’s still the best method of preventing infection and limiting transmission.”
Even if you have the vaccine you can still be unlucky enough to become ill with the flu. “Because the virus changes from one year to the next it is very hard for the experts to stay on top of it and develop a new vaccine every year in time for the annual flu season.”
However, it is not true that the vaccine can give you the flu. “The vaccine is injected into the arm but it does not contain any live virus,” says Dr Roberts. “The vaccine is made up of viral proteins and the virus cannot replicate in this and infect you because it is not contained in the vaccine.”
6) After getting the flu vaccine?
“The vaccine stimulates your immune response to protect you against an infection later on,” says Dr Roberts. “A lot of the early symptoms we associate with flu such as muscle aches and headaches are your body’s immune response to blocking infection. A mild set of these symptoms can be triggered by getting the vaccine,” she says, adding that you may also experience some soreness at the injection site.
“If a person is feeling well and healthy when getting the vaccine generally their chances of side effects in the following days are low,” says Dr O’Reilly. However, she generally advises patients to “rest up” after receiving the vaccine and avoid alcohol for 12 hours or so after receiving it so as to put no further pressure on the immune system.

7) How do we prevent the spread of the virus?
The first and most important thing to do is to get the vaccine, advises Dr Roberts. Secondly, she suggests, is always cover your mouth and nose when you cough and sneeze.
“Sneeze into your elbow or into a tissue, for example, and then dispose of the tissue and wash your hands with soap and water. Soap and water is better protection against spreading the virus than hand sanitizer.”
A practical alternative measure, suggests Dr O’Reilly, is to burn some frankincense oil in a burner. “This oil has anti-viral properties, and by diffusing it into the air around you, you can lower your risk of contracting the flu virus,” she suggests, adding that it is also a good idea to rub a small amount of the oil on your chest if you’re travelling or in contact with people who are ill as a result of the virus.
“Another alternative measure is to take Sambucol Syrup, which is distilled from elderberries and has been scientifically proven to protect the immune system against attack by the influenza virus.”
8) How the virus survives
The flu virus can survive on a solid surface for about 24 hours – for example door handles, light switches and on a soft fabric surface for up to half an hour. However, while people should definitely be aware of this form of transmission, contact transmission through objects is a lesser form of transmission – and good hand hygiene prevents it.
9) This year’s vaccine?
“There are currently four types of influenza virus that cause seasonal flu. The vaccine that is being used this year is designed to protect against all four types,” says Dr Roberts. Anyone who was vaccinated last year should understand that the 2018 vaccine is no longer relevant as two of the components of this year’s vaccine have been changed.
10) Who decides on the type of vaccine?
"Influenza experts at the World Health Organisation decide in February which strains of the virus will be used to make that year's vaccine," says Dr Roberts. "This year there was a delay in the 2019 vaccine because the WHO delayed the decision after realising that one of the four virus strains was changing. Experts had to wait for more information to allow them to predict, with maximum accuracy, which virus to include in the vaccine."

11) Popular myths about the vaccine
– Some patients believe the vaccine can give you the flu, says Dr O’Reilly. “However, the vaccine does not contain live virus so you cannot get the flu from it.”
– Some patients assume that last year’s vaccine will continue to protect them this year – it won’t, says Dr Roberts.
– Some people automatically assume they’re strong and healthy and don’t need the vaccine, says Dr O’Reilly. However, she emphasises anyone who regularly comes in contact with other members of the public should consider vaccination.
“If you are a normally healthy individual but one who is in regular daily contact with large numbers of other people in a confined space – for example teachers, dentists, office workers, the self-employed, or students – you should get the vaccine even though you may assume that you don’t need it. GPs see many otherwise healthy young people who become very ill as a result of the flu.”
12) How the vaccine works
The four virus strains that have been selected to make this year’s vaccine are specially grown in laboratory conditions. “They are then inactivated and purified so that only specific viral proteins are used to make the vaccines,” says Dr Roberts. “These proteins are injected into the body to stimulate a protective immune response so that your body makes antibodies that will then identify and bind to any incoming influenza virus that you are exposed to – and prevent infection.”
13) How quickly does the vaccine take effect?
The vaccine starts to work about two weeks after you receive the injection, so it is critical to get it early in the season.
14) Where can I get the vaccine and how much does it cost?
According to Boots’ research, about 66 per cent of people go to their GP for the service, with one in five availing of the service from a pharmacy. The vaccination process generally takes about 20 minutes because health personnel have to ensure you do not experience an allergic reaction, according to Dr Roberts, who says, however, that this is very rare.
Although the vaccine is free from the HSE, prices range from €20 in some GP clinics or from pharmacies, to up to €50 from other GP clinics. The vaccine is free of charge for those over 10 years old who are in the categories for whom vaccination is strongly recommended and have a Medical Card, Doctor Visit Card, Health Amendment Act Card (HAA) or the 2015A card which is issued under the Redress for Women Resident in Certain Institutions Act 2015.









