What is it and who gets it?
Epilepsy is the most common serious neurological condition, affecting about 45,000 people in Ireland and 50 million people worldwide.
What are the symptoms and how is it diagnosed?
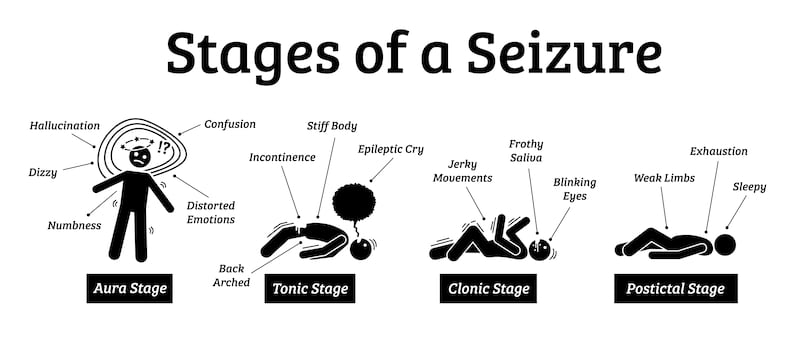
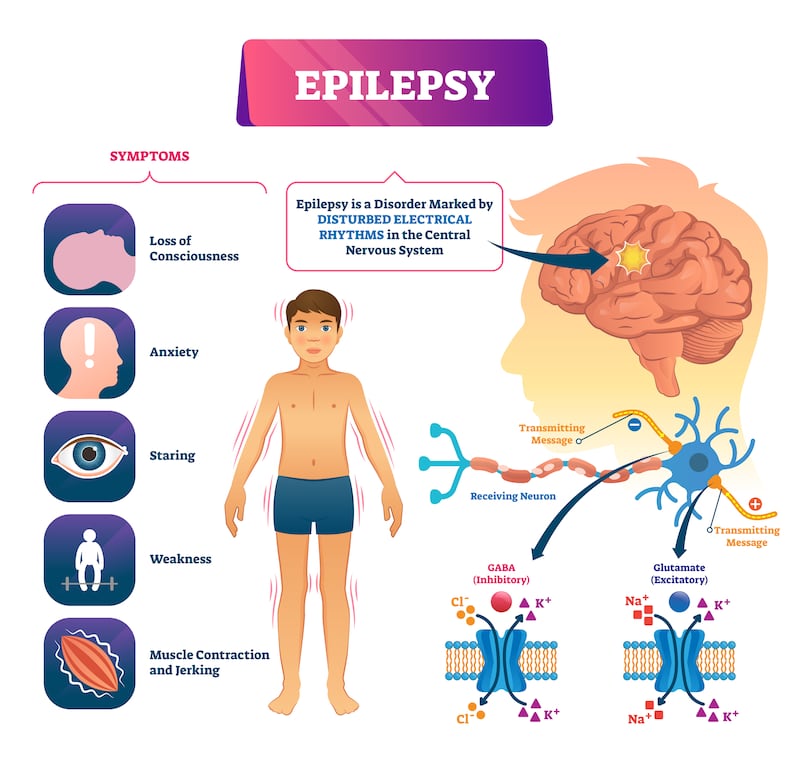
Recurrent, spontaneous seizures caused by disrupted electrical activity in the brain are the most common and recognisable symptoms of epilepsy. “Epilepsy is diagnosed following at least two seizures separated by 24 hours, however, it can be diagnosed after one seizure if electrical activity in the brain picked up by an electroencephalogram (EEG) shows further signs of another seizure,” explains Prof Colin Doherty, professor of epileptology at the School of Medicine at Trinity College Dublin (TCD) and neurologist at St James’s Hospital, Dublin. During a seizure, the individual may experience stiffness, twitching, jerking or shaking in parts of the body, blank stares, rapid blinking or other visual disturbances and sudden intense emotional and physical sensations.
Diagnosis involves a neurologist taking a medical history and analysing electrical activity in the brain with an electroencephalogram (EEG). According to Prof Doherty, there are three peaks in epilepsy diagnosis. “In infancy, where febrile seizures are very common, but only about 5 per cent of babies with these febrile seizures will go on to have epilepsy; in the 12-20 age group, which can result from a bad head injury or underlying febrile convulsions which aren’t obvious at diagnosis, and in the 50-80-year-old age group when the seizures are linked to a stroke, brain tumour, cardiovascular disease or cerebral vascular disease.”
What treatments are available and how do they compare with treatments in the past?
About two-thirds of people diagnosed with epilepsy can be successfully treated with medication, although the dose and type of medication may vary and should be monitored. About one-third of people with epilepsy have seizures that are resistant to drug therapies and about one-third of these patients may be suitable for surgery to control their seizures.
READ MORE
“Patients who are resistant to anti-seizure medicines and whose epilepsy has a disabling impact on their lives should be referred to epilepsy monitoring units at Beaumont Hospital or Cork University Hospital,” says Dr Ronan Kilbride, a neurologist specialising in epilepsy at Beaumont Hospital and the Mater hospital and the HSE clinical lead for the national clinical programme for epilepsy.
If epilepsy arises from an identifiable area of the brain that is surgically safe to remove, a patient who hasn’t benefited from two or more medicines is likely to be a suitable candidate for surgery. The most common type of surgery for epilepsy is temporal lobectomy in which the surgeon removes the part of the temporal lobe where the seizures originate. Up to 70 per cent of patients who undergo this surgery are seizure-free two years after the surgery. Vagal nerve stimulators are another type of surgical procedure that can be used to reduce seizures in children with epilepsy and intellectual disability. Other surgical options include corpus callosotomy in which a band of fibres (the corpus callosum) is cut, stopping nerve signals moving between the two hemispheres to prevent seizure activity from spreading.
A ketogenic diet high in fat with moderate amounts of protein and very little carbohydrates is another long-standing treatment for epilepsy. This diet forces the body to burn fat instead of glucose for energy, which has an anti-epileptic effect. “It is well established and should be more widely used as it works for about one-third of patients who try it,” explains Prof Doherty.
However, such diets require careful monitoring with specialist dietitians to prevent side effects. In Ireland, the ketogenic diet is most commonly prescribed for children with epilepsy and Laura Healy, who works in St James’s Hospital, is the only dietitian specialised in the ketogenic diet for adults with epilepsy. “One in three people have a 50 per cent reduction in seizures, but even those who don’t have less seizures, are more alert and more engaged on this diet,” says Healy. Some people with epilepsy benefit from a low glycaemic index (GI) diet, which is a diet low in refined carbohydrates.
Are there any particular life strategies that people with epilepsy should have?
“Sleep is really important. Other lifestyle factors are to keep physically fit, to keep your weight down and to be careful with alcohol consumption,” says Dr Kilbride. While alcohol depresses brain activity, the risk is that a person with epilepsy could have a seizure when the brain becomes excitable again when the effects of alcohol wear off.
Have there been any recent breakthroughs in treatment for epilepsy?
“The biggest shift has been the understanding that the vast majority of epilepsy cases have a genetic cause. A small number are single gene disorders but most cases are complex genetic disorders,” says Prof Doherty. Specialist epilepsy centres in St James’s Hospital, Beaumont Hospital and Cork University Hospital now use blood tests to identify the genes involved. However, many so-called precision medicines for treating the condition at a genetic level are still under development.
[ ‘Ground-breaking tech’ developed in Cork could treat drug-resistant epilepsyOpens in new window ]
Another breakthrough is a discovery by researchers at TCD that disruption to the network of capillaries in the blood brain barrier is a key driver for seizures. These findings suggest that designing medicines aimed at stabilising the integrity of these blood vessels may hold promise in treating patients who are currently non-responsive to anti-seizure medications.
The use of robotics at Beaumont Hospital to implant electrodes in the brains of patients to understand whether certain patients are suitable for surgery is another recent advance in the care of epilepsy patients that improves safety.
What are the health services like for people with epilepsy?
The HSE national clinical programme for epilepsy in 2010 followed by the model of care in 2016 created a framework for integrated care of patients with epilepsy in which hospital and community-based doctors and advanced nurse practitioners work together with patients.
“Ideally, every person with epilepsy and their GP should have epilepsy specialist nurses in regional epilepsy clinics who can advise when issues arise in their care,” says Dr Kilbride. A shortage of neurologists and advance nurse practitioners continues to be a problem for people with various neurological conditions including epilepsy and there are long waiting lists for inpatient and outpatient care.
According to Dr Kilbride, other critical areas of care needs are for women with epilepsy who become pregnant and individuals with intellectual disability and epilepsy who benefit more from care at outreach clinics rather than in acute hospitals.
What does the future hold for people with epilepsy?
Prof Doherty believes the treatment of people with epilepsy will be transformed in the next decade with better understanding of the genetics of the disease and new medicines repairing the blood brain barrier. He is also excited about research into the immune system response that could be causing the damage to the blood brain barrier, resulting in seizures. “The gold treatment in the future will be precision therapies based on current research,” he says.
It is estimated that there are about 130 epilepsy-related deaths each year, of which 20-30 per cent are deemed to be Sudden Unexpected Deaths in Epilepsy (SUDEP). Research supported by Epilepsy Ireland is investigating epilepsy-related deaths in Ireland.
“In 2024, this research will give us accurate data on the scale of the problem in Ireland and hopefully become a catalyst to develop a national strategy to reduce epilepsy-related deaths and SUDEP in Ireland,” says Paddy McGeoghegan from Epilepsy Ireland. There are also plans to introduce a safety checklist and phone app to aid doctor-patient discussion on epilepsy risks and provide people with epilepsy the tools to effectively manage their risk.




















