
Although the controversial Women’s Health Initiative – a large US study that began in 1998 – linking hormone replacement therapy (HRT) to an increase in breast cancer turned out to be flawed, the perceived risk of HRT still lingers for many, particularly women where there is already concern about breast cancer due to a family history.
And when you do go looking for reassurance on the topic, opinions and advice can be conflicting, to say the least. My mother was diagnosed with breast cancer at the age of 50, and died of endometrial cancer at 56. When my sister went to a GP in Dublin at the age of 50 with menopausal symptoms, including hot flushes and insomnia, she was immediately prescribed low dose HRT and assured she would not be at any increased risk of breast cancer.
However, when I went to a GP in Cork this year, shortly before I turned 50, complaining about debilitating brain fog, she was far more concerned about my family history and said I would be at an increased risk of breast cancer. She did agree to give me a prescription for combined HRT, but advised me to come off the medication after three months if I didn’t see an improvement in my symptoms.
There are different types of HRT, which is a treatment used to relieve symptoms of menopause – such as hot flushes, night sweats, mood swings, vaginal dryness and reduced sex drive. The medicine can come as a tablet, skin patch, gel, cream or pessary.
READ MORE
Confused and concerned about the difference in advice, I decided to make an appointment with a specialist menopause clinic, which was harder than I expected as they are few and far between in this country. After a three-month wait, I had my virtual appointment at Menopause Health in Dublin with Dr Ciara McKenna, a GP with a special interest in menopause, who was able to put my mind at ease about going on HRT.
Currently, there is no strong evidence for an additive effect of HRT upon risk of breast cancer in women with a family history
— Dr Ciara McKenna, a GP with a special interest in menopause
“As breast cancer is such a common disease, so many women have family members affected by it,” Dr McKenna says. “When you’ve seen a loved one go through a diagnosis of breast cancer, treatment and potentially a bad outcome, it’s understandable that it would be on your mind and something you would be fearful of, but most women with a family history will not be diagnosed with breast cancer themselves and HRT is not any more dangerous for them than for a woman without such a history.”
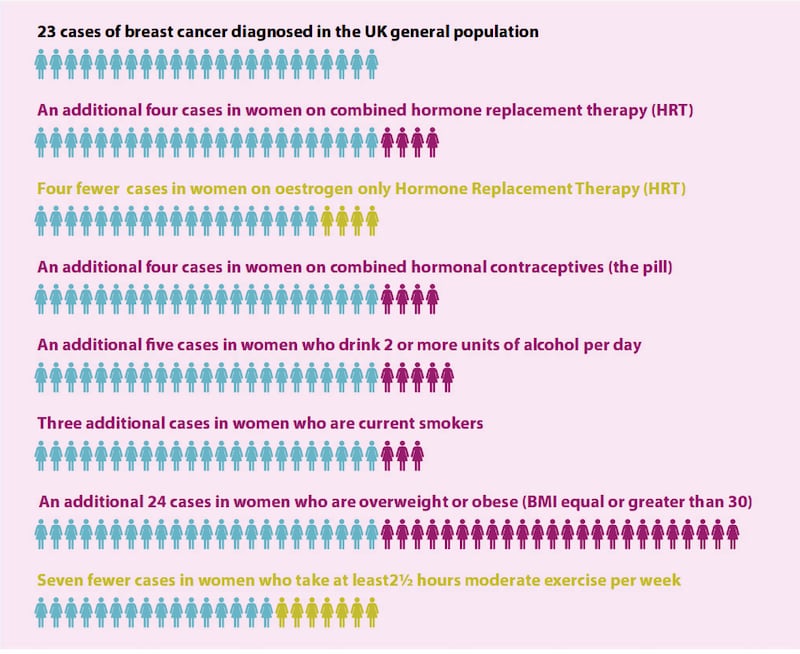
While HRT is associated with an increased risk of breast cancer in all women, Dr McKenna points out that this risk is very low – although being obese or overweight puts you at a much higher risk.
Pointing to the British Menopause Society guidelines, she says that while myself and my sister have a slightly higher baseline risk compared to somebody with no family history of breast cancer, there is no evidence that taking HRT will further increase our risk.
“Family history of breast cancer influences a woman’s baseline risk of developing breast cancer. This is affected by the number of relatives with breast cancer, the age they were at diagnosis, first degree versus second degree relative, etc. Currently, there is no strong evidence for an additive effect of HRT upon risk of breast cancer in women with a family history – ie the increase in risk relating to HRT is the same as for women without a positive family history.
“However, a woman’s baseline risk of developing breast cancer needs to be taken into account when deciding about hormonal treatment. In many women with a family history of breast cancer, their risk of developing breast cancer in their lifetime is still low and therefore the benefits of HRT will outweigh the potential harm.”
[ Majority of women can’t name any sign or symptom of common cancerOpens in new window ]
[ Menopause: ‘We are finally putting women’s health at the top of the agenda’Opens in new window ]
Dr McKenna says it is important for women to know that HRT is not the only treatment option available. If someone wants to avoid hormonal treatment or if the risk of HRT is deemed to outweigh the benefit, there are still many other effective approaches to managing symptoms, including changes to lifestyle factors and non-hormonal prescription medications.
As oestrogen stimulates the lining of the womb to grow, which could potentially lead to cancerous changes, progesterone is also prescribed – combined HRT – to balance out this risk. Due to my mother’s history of endometrial cancer, Dr McKenna explains that I would have a lower threshold for referral for ultrasounds in the event of heavy periods after the first three months of starting HRT which does not settle, or unusual bleeding or spotting between periods, to monitor the thickness of the lining of my womb.
Dr Genevieve Ferraris, a GP specialising in menopause at the Menopause Health Clinic based in Dalkey, explains there are software tools that can be used to categorise women with a family history of breast cancer into low, medium and high risk groups, depending on the number of first degree relatives you have, and the age they were at diagnosis.
“Having one first degree relative (mother, sister, father or daughter) diagnosed over the age of 40 means you are still in the low risk category, the same baseline as the rest of the population without a family history. A history of male breast cancer in the family puts you at a higher risk, particularly if somebody else on the same side of the family had breast cancer. Another high risk factor is if a relative has ovarian cancer and somebody else on the same side of the family had breast cancer.”
A number of private clinics have been set up over the past few years, but the demand from women is so high that some have a waiting list of at least three months, while others have closed their lists
After the release of the findings of the Women’s Health Initiative study in 2002, which suggested that HRT “caused” breast cancer, there was a worldwide panic and HRT use fell off a cliff. Dr Ferraris says even though the findings have since been largely debunked and HRT can reduce the risk of heart disease (a far bigger killer of women than breast cancer) and osteoporosis, the fallout still lingers and some GPs remain reluctant to prescribe HRT to low risk patients.
“I would advise any woman with a family history who is concerned about going on HRT to talk to their primary healthcare provider first, whether that’s their GP or a menopause specialist. They can get risk stratified to establish if they are at a low, medium or high risk for HRT. Some women may already be attending a specialist family history clinic and they can also seek advice about HRT there.”
There are specialist HSE menopause services at Holles Street and the Rotunda hospitals in Dublin, and a new clinic recently opened in Galway, where GPs can refer women with more complex symptoms, or with a family or personal history of cancer. A number of private clinics have been set up over the past few years, but the demand from women is so high that some have a waiting list of at least three months, while others have closed their lists.
[ Today is the day I run out of HRT patches. Consider yourself warnedOpens in new window ]
Loretta Dignam set up Ireland’s first specialist menopause clinic, the Menopause Hub in Mount Merrion, four years ago after suffering with debilitating symptoms for years before she was finally put on HRT that “changed my life”. She opened a second clinic in Santry a few months ago, which had a waiting list before it even opened, such is the demand for consultations. Both clinics are booked out until at least April, which Ms Dignam doesn’t feel is “a good enough service” and she is trying to get more GPs on board, but even the training programmes for GPs and registrars run by the British Menopause Society are booked out until next September.
“Because of Covid, we were able to move online, offer video consultations and have prescriptions sent straight to phones so women don’t have to travel to Dublin, but I’d love to have a clinic in every major urban centre,” Ms Dignam says.
The Irish College of General Practitioners recently launched a new Quick Reference Guide (QRG) to guide GPs in the management of menopause. It provides advice on diagnosis, lifestyle interventions, prescribing HRT safely, alternative options, and specific advice for women with a history of breast cancer.
However, with the enormous pressure GPs are already under, Ms Dignam says she is hearing very mixed reports about their experience when they go to their doctor complaining of menopause symptoms. “Our initial consultation is 30 minutes. We ask women to complete a questionnaire in advance, which includes their medical and family history, symptoms, smear history and whether their mammograms are up-to-date. I don’t think it’s possible to do this properly in 10 or 15 minutes. We do a 15-minute follow-up review every three months, and then every six months.”
An appointment at a specialist menopause clinic will cost you a good bit more than a visit to your GP with prices about the same as consultant services. The fee for an initial consultation at the Menopause Hub is €180 and €90 for a review. My first consultation at Menopause Health set me back €200, and my review will be €75, but I feel it was worth it for the peace of mind it gave me about starting HRT.











