If life is never the same again for parents after the birth of a child, how much more profound is the impact of the death of a child. Not only on their parents, siblings and extended family, but rippling out to friends and strangers.
So it was with eight-year-old Kevin Dunford. His parents, Mairéad and Chuck, were never given a diagnosis for his life-limiting condition, but the lack of a label didn’t matter. He was Kevin. A long-awaited first child after a miscarriage.
He was the baby whose mother, despite initial reassurances, sensed he was not quite right and it was “time to start bargaining with the gods” when she first saw him in the special care baby unit after his delivery by Caesarean section. She puts that down to a mother’s instinct, rather than her training as a paediatric nurse.
We made a pact that no matter what the outcome was going to be, we were going to love and cherish him and give him the fullest life possible
Bringing Kevin out of the maternity unit of Mayo University Hospital in Castlebar, Mairéad recalls how they went the long way home to Ballina. “We stopped on the Windy Gap between Castlebar and Lahardane, in the lay-by up there,” she says. “We made a pact that no matter what the outcome was going to be, we were going to love and cherish him and give him the fullest life possible.”
READ MORE
“The best advice we got,” says Chuck, “was from Mairéad’s aunt Geraldine: ‘hugs and kisses’, and she was right, ultimately that’s what it boils down to in the end.”
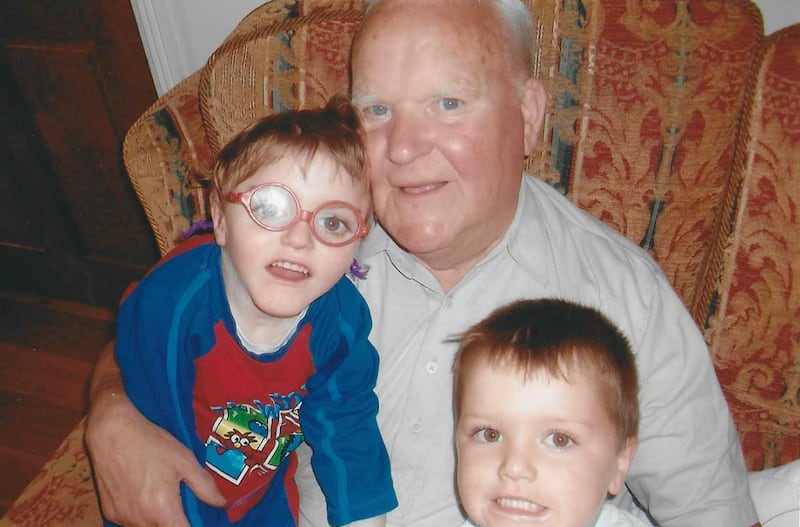
Non-verbal but engagingly communicative wide-eyed Kevin taught them to enjoy the moment. They talk of his great sense of fun and mischief, despite all the medical care he endured. They had “magical holidays” with him and the siblings that followed, Iarla, now aged 15, and Hannah, who is 13. Those that encountered him in the neighbourhood still talk of his big smile. “For a lot of people who came in contact with him, initially you’d see a boy in a wheelchair,” says Mairéad. “But within a few minutes of meeting him, then you’d see the character.”

He was no fool either. “If somebody met him, sidestepped him or treated him in that old-fashioned disability way,” she continues, “the next time he would meet them, he would turn himself in the wheelchair away from them.”
“We often say when he was alive, even though we were going 24/7, we were always happy. In the photographs, everybody’s smiling,” says Chuck, principal of Templemary National School. “You cut through all the bulls**t in life.”
Eight years on, they are sharing bittersweet memories as they talk about four close bereavements that rocked their family and the role hospice care played. They naturally dip in and out of black humour in the telling but, mindful of other people’s sensitivities, censor it as they go along.
The common denominator is the support from hospice. We would have been lost without them
It was like “compounded grief”, says Mairéad, “one death after another, after another, after another”. These included three Kevins – Mairéad’s brother, son and father, in that order – and most recently, last year, Chuck’s brother Steve.
“The common denominator is the support from hospice,” says Mairéad of both the local Mayo Roscommon Hospice service and that of the children’s hospice LauraLynn, 250km away in Dublin. “We would have been lost without them.”
When it got to the point that the family needed more than the “very supportive” disability services could offer Kevin, the couple were open to the idea of palliative care. “We had it worked out in our own heads that we needed to move into this realm. Even though it was difficult when we heard it, we were happy.”
Not only was LauraLynn there for them in Dublin, for respite and support, but they hadn’t realised the local hospice homecare team dealt with children too. It was the start of a relationship with services that continues to sustain them to this day.
They had personal assistants who had been attending Kevin for many years, and they were also getting some help from Jack & Jill nurses, but the arrival of a “fabulous” hospice nurse gave them new clarity at time when they were exhausted. She was “great fun, she didn’t come in all maudlin”, says Mairéad. “But she could do the ‘let’s get down to the serious bit’ as well.” A social worker on the hospice team also persuaded them that, yes, their family was “deserving” of a trip from the Make a Wish Foundation, and they all headed to Disneyland Paris – another precious memory.
Kevin had been in palliative care for nearly a year and a half when his beloved godfather Kevin jnr Loftus, Mairéad’s brother, “a gorgeous man”, became seriously ill with pancreatic cancer. “It was a kind of balance – who do you go to,” she says, as her son was getting very ill too, but they were used to him rebounding. On a memorable evening in March, 2014, when Chuck had brought Kevin to Mayo General Hospital to be assessed, the couple then took him to the floor below to see his godfather who had been admitted. Mairéad’s brother died there the next day, at the age of 46.
Reeling from this loss, the day afterwards Mairéad was out with her brother’s family in Crossmolina when Chuck called to say she really needed to come to Kevin in Mayo, more than 30km away. “The consultant rang me a few miles outside Castlebar and she was ever so calm, ‘Where are you now Mairéad?’, I knew she was ringing me because we’re in bother.”
Kevin was transferred to Children’s Health Ireland at Crumlin that night. Within a month he was gone too, just short of his ninth birthday. A death both expected and unexpected. They had three plans of action, if A, B, or C happened, but Kevin didn’t conform to any of them.
“He started going downhill at half eight or nine in the morning,” says Mairéad, who was there alone, as Chuck was in Mayo. “We had the ambulance waiting at Crumlin to transfer him to LauraLynn so he could die out there, because that was one of our plans if we got the sign that his time was definitely, definitely up.”
You’re thinking, He has been under palliative care for a year and a half, how could you not believe it was happening. But I couldn’t
Yet, “I couldn’t believe he was dying that morning. You’re thinking, ‘He has been under palliative care for a year and a half, how could you not believe it was happening’. But I couldn’t.”
Until, about an hour before he died, she remembers looking across Kevin’s bed at the palliative care consultant, Dr Mary Devins, and saying: “Mary, he’s not going to make it out to LauraLynn. I don’t want him to die on the M50, just cancel the ambulance.”
“The decision was made and we turned on The Beautiful South”, some of Kevin’s favourite music. Afterwards, the family were able to have his body transferred to the Butterfly Room in LauraLynn. It gave them invaluable space and time to be with Kevin, especially for seven-year-old Iarla, who at one stage asked to be left alone with him. He came out to say his big brother needed socks, which he then put on before climbing on to the bed with him. Mairéad is so grateful that her wise father had used the aftermath of her brother dying, at a time of great turmoil for her, to give his grandson “the gift of not being afraid of death”.

Not long afterwards, her father, who was in his mid-80s and living with them by then, began to experience a worsening of his prostate cancer. When Mairéad broached the subject of bringing in the hospice homecare team, “he was looking at me saying, ‘Sure I’m not dying yet’. I said, ‘No, you’re not dying, you’re up and mobile … but we can prepare’.” She reminded him how they had discussed her mother’s death from breast cancer and how hospice care, which she didn’t have, would have been good for him as well as for her.
“He thought about it then and said, ‘So I don’t have to wait until I’m dying?’ And I said, ‘No, you don’t have to wait until you’re dying, we can get them in now’. He said, ‘Grand, sure, give them a ring’.” They were delighted when the same homecare nurse who had attended to them during their son’s palliative care arrived at the doorstep, asking for “her mug” that had been well used last time round.
At that time in 2016, the Mayo Roscommon Hospice’s 14-bed centre in Knockaphunta, Castlebar, was yet to open. Would we, Mairéad muses, have done something differently if it had? “No, I think it would have still been the homecare team for dad.” However, it all comes down to circumstances and, ultimately, symptom management.
Once you drive into the grounds of that Mayo Roscommon Hospice in Castlebar, there is a sense of peace
After Chuck’s brother Steve was diagnosed with lung cancer, he was open to hospice services quite early in his illness. This means the homecare team have the groundwork done before somebody might move into the hospice, says Mairéad, who thinks people tend to leave it too late to contact them. That’s a message she wants to get out not only to families facing a significant diagnosis but fellow health professionals. She knows people are afraid to suggest it.
“It’s very brave the professional who does it, but actually we need more of them to do it and we need more of them to do it earlier. That is why we do these interviews.” Nobody ever knows when the need for hospice care is going to come to their door.
For Steve and his family, “it was a smooth transition”, she says, between homecare and the hospice unit that had opened in 2019. “It was super,” says Chuck simply, of both the staff and the building where his brother spent three weeks before his death in September 2021, at the age of 63. “Once you drive into the grounds of that Mayo Roscommon Hospice in Castlebar, there is a sense of peace.”

An author, artist, musician and historian, Steve Dunford was one of those “larger-than-life characters”. The hospice facilitated long visiting hours for family and friends who came to enjoy his company for one last time. There was a patio outside his room where he could sit in the fresh air, says Chuck, listening to the birds, the sun on his face, and he could have a visitor stay overnight.
Yet, children’s grief comes at different milestones, “it’s like they revisit the grief and have to reprocess it”. In the case of their daughter Hannah, who has Down syndrome, it was two or three years before grief came to the fore. The Dunfords didn’t know where to turn for help, being unable to access anything through the disability services. “And Mayo Roscommon Hospice stepped in again and did play therapy with her.”
Mairéad knows now she can always pick up the phone to the hospice to talk to somebody who really understands bereavement and childhood grief but who also understands that as Chuck and Mairéad’s other children grow, that creates a distance for them between Kevin and the family. After ringing to check if something is okay with one of her children she has realised, on reflection, that during the conversation it was her who was being reassured that she was okay.
As she and Chuck too will sometimes reaffirm with each other, after all they’ve been through, “we’re doing all right”.
On Sunday, November 27th, Mayo Roscommon Hospice Foundation will hold their annual Shine a Light Christmas tree lighting ceremony at Knock Shrine. Lights can be sponsored on the tree for €5 each. All proceeds go towards funding palliative care services in the communities of Mayo and Roscommon.
Panel
A community hospice service by numbers
- 17 nurses work on the palliative homecare teams in Mayo and Roscommon.
- 44 per cent of the costs are funded by the Mayo Roscommon Hospice Foundation.
- €15 million, all fundraised, was the cost of building two hospice units. The Mayo centre opened in 2019, the Roscommon unit will open to patients in the next few weeks.
- €2 million has to be raised each year towards the running of services; the foundation does this through 12 charity shops and other fundraising.












